This post is my attempt to get my head around insulin resistance; what it is, what happens and why. I’m trying to get a handle on the mechanisms involved and explain it in as simple terms as possible in a way which makes sense. The problem is that biological pathways are complicated. So complicated that I end up getting a little bit of the story and thinking that I understand things. Would you care to join me in the journey?
Because I learnt a lot researching this I hope that you find it useful. However please don’t expect the ultimate explanation because it has had to be simplified!
24/7 service. No days off.
We are starting this journey with a recognition that the cells in our body never take a break. We may sleep allowing our body to renew and repair, body processes keep going. Hearts keep beating, kidneys filtering, livers do a huge number of things and they are not working alone.
So our cells require a constant stream of energy from a number of sources. Glucose from carbohydrates, fatty acids from fats and amino acids from protein. Glucose and fatty acids being the most important. All cells can utilise glucose while cells with mitochondria can use other sources.
Cells with mitochondria.
Cells with mitochondria take pyruvate (made by splitting glucose), fatty acids or amino acids and turn them into energy packages called ATP. Pyruvate and amino acids each give about 40 ATP per molecule. A fatty acid molecule turns into 100ATP. The process is called the Kreb’s cycle or the citric acid cycle. It is a series of reactions, steps, each generating ATP.
These mitochondria are remnants of bacteria which were incorporated into cells millions of years ago. It was an inovation which allowed life forms to get going and move out of the primordial soup. Mitochondia gave cells an evolutionary advantage but surprisingly not all have them.
Cells without mitochondria.
These cells can only utilise glucose for energy and they do that in the cytoplasm where glucose is split into two pyruvate molecules. If you get a quiz question about this – the major cells that do not contain mitochondria are red blood cells. They also don’t have a nucleus.
Role of the pancreas.
Like the liver, kidneys, heart etc., the pancreas is another very hard working organ. It has two main functions – producing and releasing enzymes to break food down into glucose, fatty acids and amino acids and also to regulate the levels of glucose in the blood.
Glucose is essential fuel for cells but it is also toxic in the bloodstream. Complications of diabetes occur in cells which can’t protect themselves from all the glucose (blindness, nerve damage, heart disease to name but 3) so the pancreas has to keep the balance just right with insulin and glucagon.
Insulin and glucagon.
Insulin is released to lower glucose levels after a meal. It shuttles the glucose into cells for imediate use, muscle cells and the liver for storage as glycogen and the fat cells to be stored as, well, you guessed it, fat.
Once all the glucose has gone glucagon is released to tell the liver to break down glycogen and release it back into the blood for transport to cells which can only utilise glucose. Muscle cells do not release glucose back into the blood – their glycogen is broken down and used as they need it. Other cells switch to using fatty acids when glucose is needed elsewhere and muscle cells also switch to fatty acids once their glycogen stores are exhausted. This is where the guidance that you have to exercise for 20 minutes before you start burning your fat stores comes from.
Glut4.
The cells have to know what fuel to expect and the presence of insulin signals that glucose is on its way. Insulin signals to a transporter protein stored in the cell, glut4. Glut 4 is called to the cell membrane where it picks up glucose and transports it inside. Once insulin goes, glut4 goes back inside and leaving glut1 to transport any glucose that turns up. Think of glut4 as being the motorway transport while glut1 is slower.
Insulin resistance happens when glut4 stops responding well to insulin. WARNING! This is where it is tempting to pull out the smoke and mirrors, say “complicated” and move swiftly on.
It seems that insulin resistance is driven by inflammation in the body. Adipose tissue releases cytokines which drive inflammation and inhibit glut4 expression. You got it – fat cells.
Adipose tissue and inflammation.
Fat cells are part of the adipose tissue which instead of being a passive storage of fat turns out to have a vital role in our immune system. Once fat cells reach a certain point (probably different for everyone), it starts releasing proinflammatory cytokines. As a result glut4 stops responding and more insulin is required to clear the glucose.
ACE2 receptors.
We’ve heard a lot about ACE2 receptors on cells being the gateway used by covid-19 for cell entry and how people with inflammatory, lifestyle diseases have more of these receptors. Surprise! These receptors are produced to reduce insulin resistance. ACE2 gets more glut4 up to the surface.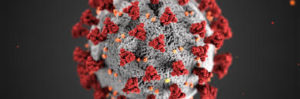
Yup – beats me too!
Further reading:
ACE2 receptors are a response to high bloodsugar level/inflammation to increase insulin sensitivity.
Coronavirus and obesity: could insulin resistance mediate the severity of covid-19 infection?




